Early schizophrenia: best practice to optimise outcomes- Highlights Pt 3 of 3
Professor Scott provided an overview of his recent publication on key pharmacotherapy principles for quality prescribing in early psychosis.1 He introduced the six key principles (Figure 1), leading with the first point that treatment decisions should be informed by medication side effects. “Antipsychotics have almost equivalent efficacy,” he explained.2,3
“The choice of antipsychotic should be guided mainly by tolerability,” - Professor Scott
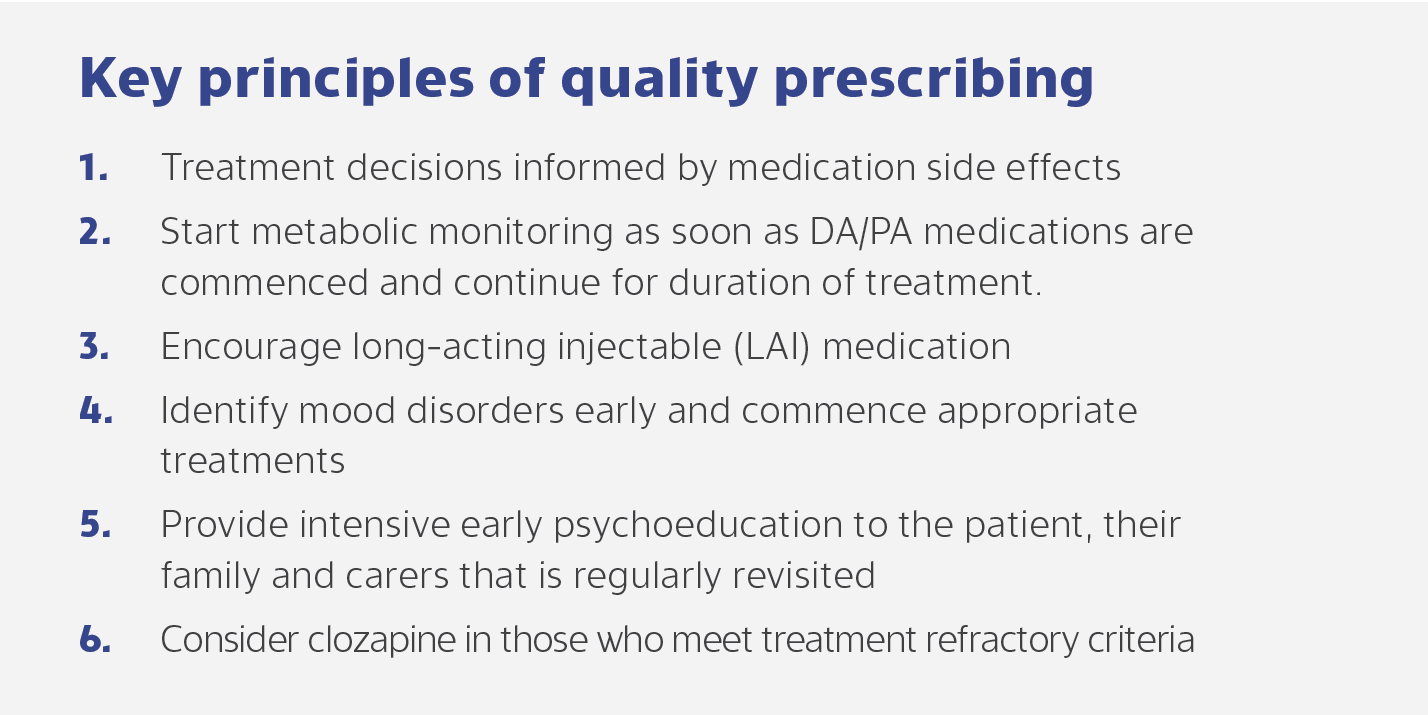
Figure 1. Key principles of quality prescribing. DA, dopamine agonist; PA, partial agonist.
Adapted from Scott et al., 20221
Figure 1. Key principles of quality prescribing. DA, dopamine agonist; PA, partial agonist.
Adapted from Scott et al., 20221
A recent network meta-analysis of 127 randomized, controlled trials including 18,152 participants found no clear differences between antipsychotics for relapse prevention (Figure 2).3 Similarly, a network meta-analysis of 92 randomized, controlled trials including 22,645 participants showed that most oral and long-acting antipsychotics were effective for relapse prevention in schizophrenia-spectrum disorders.2 The message for relapse prevention is thus the same as that presented by Professor Leucht for acute schizophrenia: “The choice of antipsychotic should be guided mainly by tolerability,” Professor Scott summarised.
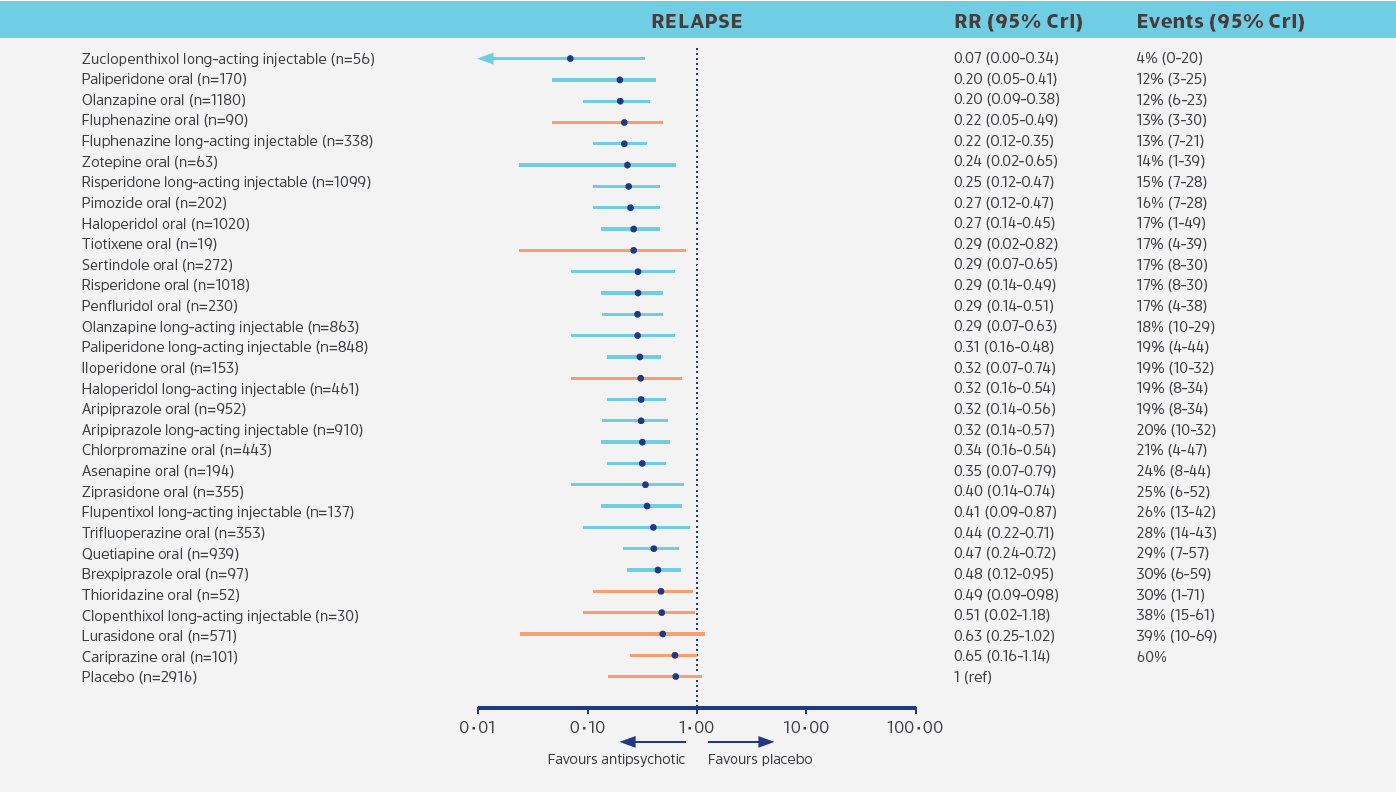
Figure 2. Oral and long-acting antipsychotics for relapse prevention in schizophrenia. Adapted from Schneider-Thoma et al., 20229 Note: not all listed antipsychotics are available in Australia. CI, confidence interval; RR, risk ratio.
Figure 2. Oral and long-acting antipsychotics for relapse prevention in schizophrenia. Adapted from Schneider-Thoma et al., 20229 Note: not all listed antipsychotics are available in Australia. CI, confidence interval; RR, risk ratio.
Encouraging long-acting injectable (LAI) medication was another key principle of quality prescribing presented by Professor Scott. Evidence on the superiority of LAIs compared with oral antipsychotics comes from both clinical trials and real-world evidence.4,5 In a randomized clinical trial, use of a LAI antipsychotic reduced relapse rates and improved adherence compared with the equivalent oral antipsychotic.4 A real-world study from Sweden that followed up 29 823 patients with schizophrenia for a median of 6.9 years observed that 44% patients of patients were rehospitalized.5 The lowest risk of rehospitalization during monotherapy was observed for patients treated with LAI antipsychotics or clozapine compared with no use of antipsychotic medication (HR, 0.78; 95% CI, 0.72-0.84 in the total cohort).5 LAI antipsychotics substantially reduced the risk of rehospitalization compared with equivalent oral formulations.5
LAI antipsychotics substantially reduced the risk of rehospitalization compared with equivalent oral formulations.5
How long should patients stay on medication? Clinical studies in schizophrenia tend not to be longer than 2 years, but that is not evidence that this is a good time to stop, Professor Scott explained. Research highlights that there are high rates of relapse if patients discontinue their medication. A review of randomized, controlled trials in first episode psychosis found higher rates of relapse in patients undergoing dose reduction or medication discontinuation than in those with treatment maintenance.6 When patients relapse, this contributes to treatment resistance. In a longitudinal follow-up study, the proportion of patients who respond to antipsychotic treatment was substantially lower in second- than first-episode schizophrenia, even though all patients received the same antipsychotic for both episodes.7
“The one thing all psychiatrists can do is excellent medication management,” Professor Scott reiterated in conclusion to his presentation.
Presented by Professor James Scott, Head of Child and Youth Research Group at QIMR Berghofer Medical Research Institute, and Director of Early Psychosis at Metro North Mental Health Service. Session chaired by Professor Nagesh Pai.
The symposium on Data, Discussions and Decisions in Psychiatry was held in Sydney (14 May 2022). The programme included clinically focussed sessions and expert panel discussions on treating people with schizophrenia.
Our correspondent’s highlights from the Psychiatry Symposium: Data, Discussions and Decisions in Psychiatry, are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.
Internal ID: AU-HLU-0057. August 2022